Featured articles




Comment
Featured articles
MoD Matrix Agreement: Major breakthrough for thousands in military hearing loss claims
08/07/2024
Firm News
See all articles



Comment
See all articles
Private wealth dispute insights
Assisted dying law in the UK: Current legal implications and proposed new law
09/01/2026

Comment
Family law insights
Bigamous marriage: How bigamy affects marriage, divorce and children
12/12/2025

Deals
See all articles

Deals
Sports Deals
Hugh James advises OffPitch Sports International on first investment round
09/09/2025
Charities, Community, & CSR
See all articles


Charities, Community, & CSR
Firm News
Hugh James Rugby Lunch 2024 raises £29k for charity partners
15/11/2024

Charities, Community, & CSR
A memorable day in Horatio’s Garden: Treasure hunt and afternoon tea
26/06/2024

Charities, Community, & CSR
Hugh James continues to support Horatio’s Garden Wales | Nurturing the wellbeing of people after spinal injury
21/05/2024
Case Study
See all articles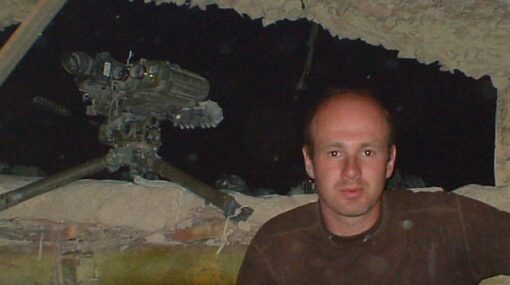
Case Study
Military case studies
Substantial settlement for soldier with noise induced hearing loss
13/01/2026

Brain injury case studies
Case Study
Serious injury case studies
Life after serious injury: Hope, recovery and purpose
18/12/2025

Case Study
Military case studies
British Army soldier secures over £700,000 following career-ending cold injury
04/11/2025

Case Study
Military case studies
Landmark settlement of £1 million (gross) for Royal Navy Veteran after non-freezing cold injury
03/11/2025
Witness Appeals
See all articles
Witness Appeals
Witness Appeal: Did you work with Ian Stoneley at Imperial Chemicals Ltd?
07/01/2026

Witness Appeals
Witness Appeal: Did you work with Mr Arthur Mott at Hotpoint in the late 1960s?
04/12/2025

Witness Appeals
Witness Appeal: Did you work with Mrs Christine King at West Cornwall Hospital in Penzance
01/12/2025
Witness Appeals
Witness Appeal: Did you work with Dennis Baxter at Apex Insulation or London Regional Transport?
13/11/2025
Witness Appeals
Witness appeal: Did you work with Mr Andrew Horton at the Inland Revenue Building in Llanishen, Cardiff?
23/10/2025

Witness Appeals
Witness appeal: Did you work with Mr Denis Tapp at a Dockyard in Plymouth?
07/10/2025







